Clinic
Headache
As compassionate caregivers, we help patients achieve a level of relief that can improve their quality of life.
Dr. Martinez and our team of highly-educated physician assistants and nurse practitioners are specialists in Headache, Traumatic Brain Injury (TBI), Concussion, and Post-Concussion Syndrome with expertise in Chronic Migraines. Our goal is to provide excellent comprehensive headache care.
Once we have established the diagnosis, we develop a management plan for your specific headache type. This management plan may include patient education, preventative and acute medication trials and keeping a headache diary. The goal is to establish a headache-free state whenever possible.

Headache Acute Rescue Program
Available M – F 8a.m. – 5p.m.
Sat hours coming soon
Sat hours coming soon
Available for established patients including:
- Toradol IM injection
- Sumatriptan IM injection
- Cefaly-transcutaneous electric nerve stimulation device for migraine acute and preventative treatment
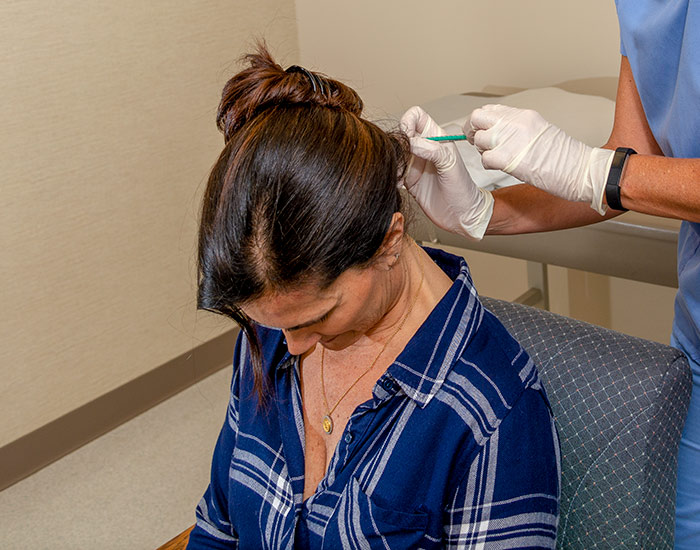
- Occipital Nerve Block — The most common nerve block procedure involving an injection in or around the nerves in the scalp over the back of the head
- Supraorbital Nerve Block — Nerve block includes injections to the face just over the eyebrow
- Trigger Point Injections — Injection is performed on and around painful area, often pointed out by patient and identified by muscles in tight knot causing a headache or resulting from a migraine.
- SPG Blocks (sphenopalatine ganglion blocks) — The sphenopalatine ganglion (SPG) is a collection of nerve cells that is closely associated with the trigeminal nerve, which is the main nerve involved in headache disorders. A nerve block is a procedure to stop pain transmission through anesthesia to the nerve. In a SPG block, an anesthetic agent is administered through the nose. The procedure is done in the office and providing sustained relief of pain allowing restored normal function.
- Anti-Nausea injection
- Ice Helmet, Hot Packs
- Medication management
Specialized care we offer:

Medication Management
Preventive medications are taken daily to prevent migraine attacks from occurring. They are not intended for use to treat an acute attack. Many different preventive medications are available, and the choice of medication depends on many factors such as co-existing conditions—including high blood pressure, asthma, diabetes, or pregnancy (among others). Therefore, choosing medications for preventive therapy can be a complex process.
Before starting to take medications, several basic principles need to be considered:
- The choice of a preventive medication needs to be tailored to meet each person’s individual needs. Co-existing medical conditions (such as depression, obesity, anxiety, among others), drug side effects, other medications being taken, and individual patient needs will help determine which medication Dr. Martinez will choose for you.
- Headache/Migraine patients do not want to suffer from an attack, so prevention is important even if they suffer from only one attack a year. Those who suffer from frequent attacks will need more aggressive prevention strategies that sometimes include medication. Additionally, nonpharmacological prevention may help if you have:
- Disabling attacks despite appropriate acute treatment
- Frequent attacks (>1 per week).
- Insufficient or no response to acute drug treatment.
- Poor tolerance or contraindications for specific acute pharmacological treatments.
- History of long-term, frequent, or excessive use of pain medications (analgesics) or acute medications that make headaches worse (or lead to decreased responsiveness to other drug therapies).
- Migraine prevention is intended to reduce the frequency, suffering and disability associated with migraine attacks. Unfortunately, preventive treatment strategies rarely eliminate migraine, but they can reduce the frequency and severity of attacks.

Types of Migraine Prevention Treatments
- Botox for Chronic Migraine — Botox (Allergan) received FDA approval for the treatment of chronic migraine in October 2010. It is used for preventing Chronic Migraines in adults who experience 15 or more migraine days per month, with headaches lasting 4 hours per day. Treatment is repeated every 12 weeks.
- Anticonvulsants or anti-epileptics
- Beta-Blockers
- Calcium Channel Blockers
- Antidepressants
- Calcitonin Gene Related Peptide antibody (CGRPab) blockers
- Vitamins, Minerals and Herbs — may also be used in the prevention of migraine. Make sure to let Dr. Martinez and your Practitioner know about all medication and supplements you are taking as some may interact badly with each other or cause serious side effects when taken together.


Current Acute Migraine Treatment Options
When your migraine symptoms begin, acute treatment is designed to be readily available, easily dosed and quickly relieve the pain and symptoms. On a perfect day, these medications should consistently ease your symptoms and keep them away for at least 24hours. As a participating physician with the American Academy of Neurology, American Headache Society and US Headache Consortium Dr. Martinez has established the following goals for successful acute treatment of migraine attacks both in and out of the office:
- Treat migraine headaches rapidly and consistently without recurrence
- Restore the individual’s ability to function
- Minimize the use of backup and rescue medication
- Optimize self-care
- Cost effective for overall management (including patient savings programs, etc.)
- Minimal or no side effects
Many different types of medication are used for acute migraine treatment:
- Triptans — regular tabs, dissolving tabs, injections, needless injections, rectal suppositories, nasal spray, nasal powder
- NSAIDS (non-steroidal anti-inflammatory drugs) Naproxen, Cambia, Toradol, Sprix
- DHE 45
- Ergotamines- Migranal, Cafergot, Migergot
Doctors recommend against using many acute treatment medications more than twice a week. More frequent use may lead to medication overuse, or rebound headache. If migraine headaches are recurring more frequently, an addition of a preventative medication may be needed.
Remember… when migraine headaches are treated early at onset of the headache with acute medication most can be stopped in their tracks with the 1st dose of medication.
Understanding the different types of migraine and headaches
More than 37 million Americans suffer from migraine, with women being affected three times more often than men. Migraines are most commonly experienced between the ages of 15 and 55; 70% to 80% of sufferers have a family history of migraine. Less than half of all migraine sufferers have received a diagnosis of migraine from their healthcare provider. Migraine is often misdiagnosed as sinus headache or tension-type headache.
When people hear the term ‘migraine,’ they often think of a severe headache. What they don’t always know is that migraine is a neurological disease and that there are a number of different subtypes of migraine. Find out about the different types of migraine below.
Please see the Education section of our Glossary page for more information and resources.
About a quarter of people who experience migraine also experience aura, a series of sensory and visual changes that can range from seeing black dots and zig zags to tingling numbness on one side of the body, or an inability to speak clearly. Aura sets in shortly before or during a migraine, and can last anywhere from 10 to 30 minutes. Aura is the second of migraine’s four stages, and anyone who experiences it will confirm it is an unmistakable warning sign that the severe head pain is on its way.
Diagnosing migraine without aura can be difficult because the symptoms are similar to several other types of migraine. Pulsing or throbbing pain on one side of the head, photophobia, phonophobia, pain that is made worse by physical activity, and nausea and vomiting are all classic symptoms of Migraine without Aura. The key differentiator is that Common Migraine lacks the warning phases (prodrome and aura) that other types of migraine have.
Also called a Silent or Acephalgic Migraine, this type of migraine can be very alarming as you experience dizzying aura and other visual disturbances, nausea, and other phases of migraine, but no head pain. It can be triggered by any of a person’s regular triggers, and those who get them are likely to experience other types of migraine, too. The International Headache Society classifies this type as typical aura without headache.
If you have ever had a migraine that felt more like a stroke, it was probably a Hemiplegic Migraine. People who experience this type of migraine develop weakness on one side of the body, often with visual aura symptoms and a “pins and needles” sensation, or loss of sensation, on one side of the body. It can last for as little as a few hours to several days. Similar to typical aura without headache, Hemiplegic Migraine doesn’t always include the severe head pain.
When a headache causes you to temporarily lose vision in one eye, it is a Retinal Migraine. Most common in women during their childbearing years, the blindness can last anywhere from a minute to months, but is usually fully reversible. This is a specific type of aura that accompanies a migraine, and it’s a condition we know very little about. What we do know is that Retinal Migraine may be a sign of a more serious issue, and those who experience it should make a point to see a specialist.
If you have a headache more than 15 days a month, you’re probably suffering from chronic migraine. Many of the days often feel like typical migraine, but there may be considerable variability in the severity of the symptoms and head pain on any given day. Some days patients may mistake the pain for a “tension-headache” or “sinus headache” if the pain is less severe. Many patients with chronic migraine also use acute headache pain medications on more than 10–15 days per month, and this can actually lead to even more frequent headache.
Ice pick headaches are pretty self-explanatory. They feel like you’re getting stabbed in the head with an ice pick. They often come on suddenly, delivering an intense, sharp pain. They’re short–usually only lasting 5–30 seconds–but incredibly painful. These headaches occur on the orbit, temple, and parietal area of your head. That’s where your trigeminal nerve is, the nerve in your face that’s responsible for biting and chewing, as well as face sensation. The nerve is on the side of your head just past your eye and above your ear. If you get sharp pains in this area, chances are you’re getting ice pick headaches.
This is one of the most severe types of pain that a human can experience. With cluster headaches, you’ll feel an almost burning pain around and above your eyes, at your temples, and even moving toward the back of your head. You’ll often also get red or swollen eyes or a runny nose, among other symptoms. Because they occur in such a large area and provoke other symptoms, cluster headaches can be the most irritating headache, and are sometimes referred to as “suicide headaches.”
When the pain in your head is actually caused by pain in your neck, you probably have a cervicogenic headache. The pain usually comes from the neck or from a lesion on the spine, which is often confused with pain in the back of your head. It’s common for this type of headache to require physical therapy in addition to medication or other treatment.
Pinpointing the cause of the headache is sometimes complicated. There are many types, and many methods of treatment. Focusing on where exactly your head hurts and the accompanying symptoms can help determine what type of migraine or headache you suffer from, resulting in a more effective treatment plan and fewer painful days.
Headache and Migraine Triggers
Many Factors can trigger migraine attacks, such as:
- Changes in sleep-wake cycle
- Missing or skipping a meal
- Medications that cause a swelling of the blood vessels
- Headache medication overuse
- Bright or fluorescent lights
- Sunlight/Environmental
- Snoring and sleep apnea
- TV and movie viewing
- Specific foods or drinks
- Excessive noise
- Excessive caffeine use
- Sexual activity
- Exhaustion/fatigue
- Hormones
- Smells/odors
- Temperature or weather changes
- Exercise
- Travel
- Alcohol
- Negative event
Stress and/or underlying depression are important trigger factors that can be diagnosed and treated adequately, as well.
Headache and Migraine Warning Signs
Migraine pain is typically felt around the eye or in the temple area. Pain can also occur in the face, sinus, jaw or neck area. Some people have tingling in their arms or face or trouble speaking. Others experience visual auras such as wavy lines, dots or flashing lights and blind spots twenty minutes to one hour before the actual onset of a migraine.
Tests such as MRI and CT scans are useful tools to confirm the lack of organic causes for the patient’s headaches.
There is currently no test to confirm the diagnosis of migraine.

Key Headache Clinic Staff
-
-
-
-
-
-
-
 Salina Gomez, M.A. Medical Assistant / Authorization Coordinator
Salina Gomez, M.A. Medical Assistant / Authorization Coordinator