Clinic
Epilepsy
Did you know that having a seizure does not mean a person has epilepsy? Many people have a single seizure in their lifetime because of an injury, illness, or fever… this is not epilepsy. Only when a person has had two or more unprovoked seizures is he or she considered to have epilepsy. A seizure is like an “electrical storm” in the brain and the normal pattern of activity is temporarily disturbed. Epilepsy is the 4th most common neurological disorder in the U.S.
Two Type of Seizure
There are 2 major types of seizure: focal seizures and generalized seizures. The type is determined by how the seizures start.
- Focal seizures (also called partial seizures) begin in just one part of the brain. The feelings or sensations a person may have during focal seizures depend on which part of the brain is affected. Partial seizures may spread to affect both sides of the brain.
- Generalized seizures result from abnormal brain cell activity on both sides of the brain at once. These seizures may cause momentary stares, loss of consciousness, falls or massive muscle spasms.
The Brain’s Wiring
The human brain is so complicated that many things can it “act up” and produce seizures. Some seizures occur because the brain’s wiring — the connections between brain cells — did not develop correctly. Sometimes it runs in families and is caused by genetic influences. But about half of all seizures have no known cause and researchers continue to learn about the many things that cause epilepsy.
Seizures rarely happen in the presence of a health care provider. Dr. Martinez and our team believe a detailed medical history is one of the best tools to lay the ground work diagnosing a patient with epilepsy and if so what type he or she has. Since many people who have a seizure can’t remember the seizure itself, it’s important for somebody close to the person to give an account of the episode.

Diagnosis with EEG
A test called an EEG may be used to diagnose epilepsy or determine the type. An EEG measures the electrical activity of the brain. Sometimes a person with epilepsy will have abnormal patterns of brain waves, an epilepsy “fingerprint.” This can help pin down a diagnosis. By itself, an EEG may not be enough to confirm a diagnosis. Not everyone who has epilepsy has an abnormal EEG and some people who never have seizures show abnormal brain wave patterns.
At the Neurology & Pain Specialty Center we offer in-office EEG services for our patients, when ordered.
Specialized care we offer:

Medication Management
Dr. Martinez and your Physician Assistant/Nurse Practitioner will work with you to determine if an anti-seizure medicine is right for you. It may take some “experimenting” to find the one that works best for you. In some patients, seizures can be best controlled by combining two or more medicines.
More than 20 different types of anti-seizure medicines are now available. Which medicine will work best for you depends on many factors including seizure type, lifestyle, age, other medications. Taking medicines exactly as prescribed is key: take the right dose, at the right time, carefully follow the directions such as whether to take with food or not.
If you have difficulty keeping track of your medicine or taking as directed, speak with your provider. Good communication is an important step in helping to get you seizures under control.
Surgical Treatment Options
When seizure can’t be controlled by medicines, surgery may provide another option for some patients. Surgery is typically not the first treatment option. It is usually considered only after at least 2–3 medicines have been tried without success.
For those patients who are candidates for surgery, a common technique is to remove a small area of the brain where seizures start. In general, people have a better chance of becoming seizure-free after surgery if doctors can figure out where the seizures are beginning.
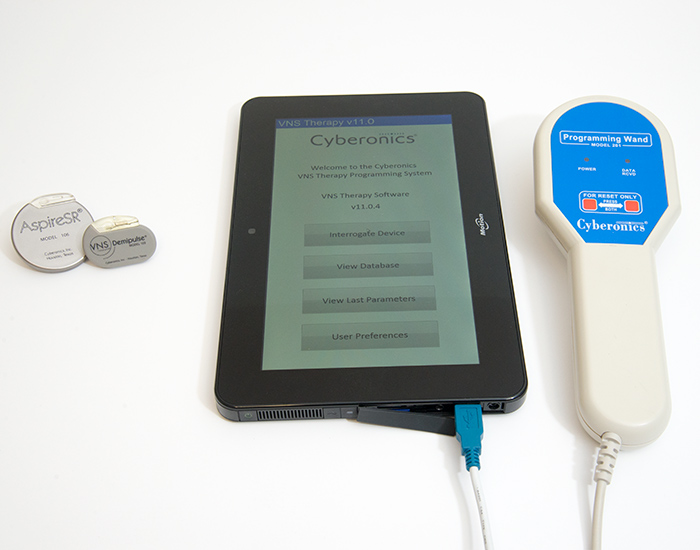
In addition to surgery another treatment option is Vagus Nerve Stimulation (VNS). Stimulating this nerve has been found to reduce epilepsy seizures in some people by 20% to 50%. The stimulator is a small, battery-powered device implanted under the skin of the chest, much like the deep brain stimulator (DBS). It connects to the vagus nerve in the lower neck.
The device delivers short bursts of electricity to the vagus nerve which in turn influences the brain. The stimulation can be either continuous or it can be controlled by the patient if she or he feels that a seizure may be about to happen.

Create Your Seizure Plan
Work with your practitioner to make your “seizure plan.” This is a list of things to do, both for yourself and any relatives or caregivers who are likely to be around you. Here are some things we suggest:
- Wear a bracelet or other ID with our medical information on it
- Consider keeping a seizure or epilepsy diary (ask us for a diary or list of app suggestions)
- Organize emergency contact numbers
- Learn to recognize auras and other seizure warning signs and take steps to move to a safe location or position
- Learn your own seizure triggers (ex: lack of sleep, alcohol, stress, hormone changes related to period)
- Safety proof your environment (pad sharp corners, use barriers to protect against hazards such as heights, pools, bodies of water, fireplaces, etc.)
Review your plan with your practitioner, relatives or caregivers of children.